Coping with chronic illness and pain can be considerably difficult. Having a long-term, chronic illness can impact almost all aspects of life. Chronic illness can be associated with a lot of difficulties, and patients need to change many behaviors as part of illness management.
Difficulties related to pain, fatigue, missed work, reproductive health and worry, uncertainty, medical treatments and procedures, relationship and family difficulties, stress, anxiety, depression, loneliness, anger, sleep difficulties, financial problems, and loss of confidence can all be hard to cope with. In fact, approximately 25% of patients with chronic medical problems experience significant psychological symptoms. Because complete illness symptom reduction is not always possible, learning strategies to cope with living with a chronic illness is important.
Behavioral Medicine
Behavioral Medicine is “the interdisciplinary field concerned with the development and integration of behavioral, psychosocial, and biomedical science knowledge and techniques relevant to the understanding of health and illness, and the application of this knowledge and these techniques to prevention, diagnosis, treatment and rehabilitation.” Behavioral Medicine is also known as “Mind-Body Medicine.” Informed by research, behavioral medicine utilizes behavioral health techniques to treat a variety of medical and mental health conditions.
biopsychosocial model of chronic illness and pain
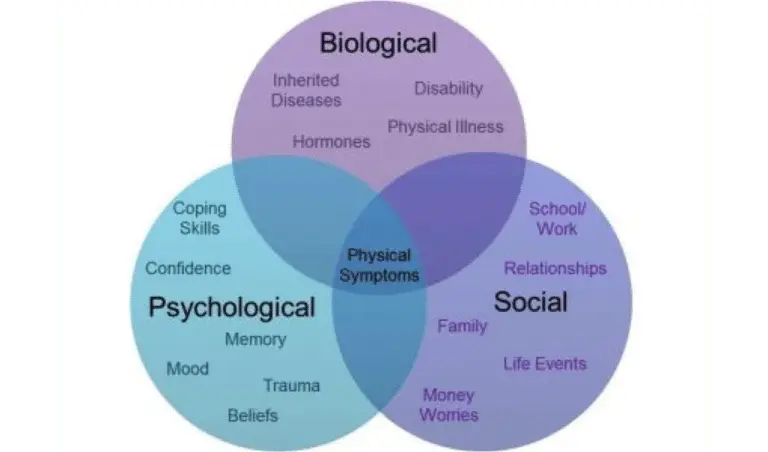
The biopsychosocial model of chronic illness and pain is a full perspective that pulls together all the aspects of the illness or pain experience. It has four primary components:
- biological
- psychological health
- social function
- physical functioning
From this perspective, we are encouraged to go beyond simply focusing on the biological aspects of illness, expanding to also include psychological and social aspects of illness. This model serves the most comprehensive way to understand and manage chronic illness and chronic pain. From this framework, it is understood that psychological factors may modify one’s perception of pain. This is not to say that psychological factors CAUSE the experience of pain.
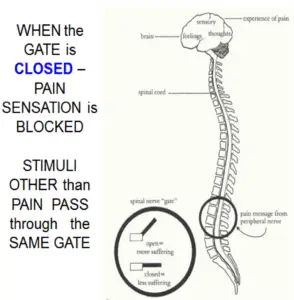
Gate Control Theory of Pain
The Gate Control Theory of Pain was developed to help to make sense of the well-known importance of the mind and brain in one’s perception of pain. According to gate control theory, the experience of pain depends on a complex relationship between the central and peripheral nervous system. It is understood that when injured, pain messages starting in nerves around the damaged region flow along the peripheral nerves to the spinal cord, and on up to the brain. Before these messages get to the brain, they go through “nerve gates” in the spinal cord that either open or close depending upon various factors. When the gates are open, pain messages “get through” and the experience of pain can be strong. When the gates are closed, pain messages are unable to reach the brain, and pain may not even be experienced.
The Pain Cycle
This pain cycle diagram can help us to describe ways chronic pain can impact a person’s life.
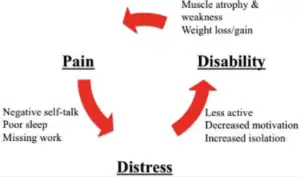
When people experience pain over an long period of time, they may develop hopeless beliefs about their pain (e.g., “I am never going to feel better” ) or negative thoughts about themselves (e.g., “I have ruined my life”). When these types of thoughts continue, people may begin to become depressed or anxious. As pain continues, they may avoid doing everyday activities for fear of further injury or increased pain, feel low motivation, and isolate themselves. As people withdraw and become less active, their muscles are likely to become weaker, they may have changes in weight, and their overall physical health may decline further.
This “Cycle of Pain” framework helps us to understand how distress and disability impact the experience of pain, and can make the pain worse.
Helpful Psychological Treatments
Several psychological treatments have been shown to be helpful towards reducing both psychological distress associated with chronic illness and pain, and towards reducing the experience of pain. Cognitive Behavioral Therapy (CBT), Relaxation Training, Mindfulness, and Motivational Interviewing have all been shown to be helpful.
Goals for Chronic Illness and Pain Management
In Cognitive Behavioral Therapy (CBT) for chronic pain and illness, a client works with a Behavioral Medicine-trained psychologist to accomplish the following goals:
- Identify and treat (or manage) underlying illness
- Increase productivity and functioning
- Reduce the incidence and severity of pain
- Reduce emotional or psychological distress
- Improve quality of life
These goals are accomplished by:
- Empowering clients through education, support and encouragement.
- Promoting healthy lifestyle behaviors.
- Developing specific strategies to manage pain and/or reduce distress.
Cognitive Behavioral Therapy in behavioral medicine
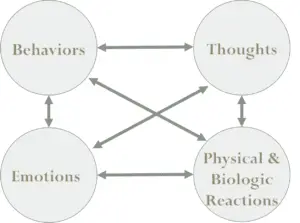
Cognitive behavioral therapy in Behavioral Medicine works to address the interplay between thoughts, behaviors, emotions and physical reactions to reduce distress.
We know that all of these pieces work together. That is:
- What we think affects how we act and feel psychologically and physically.
- What we feel psychologically and physically affects how we think and what we do.
- What we do affects how we think and feel psychologically and physically.
And as Gate Control Theory helps us to understand, our mood and thoughts can significantly impact also our experiences of pain.
Even without clear psychological difficulties, those with chronic illness and chronic pain have to cope with oftentimes complex thoughts, feelings and behaviors.
Let’s use an example to demonstrate:
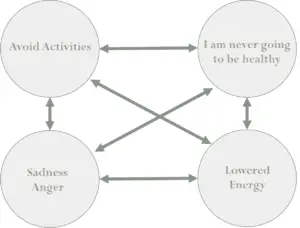
Thinking “I am never going to be healthy,” or “Nothing I do makes any difference” is likely to contribute to increased sadness and anger, and is also likely to increase avoidance of activities. This in turn, will lower energy levels, which further depresses our mood (and so on).
As you can see, this model helps us to understand how the thoughts, behaviors, moods, and physical reactions that we have each tend to contribute to the other components in the model.
Behavioral Medicine CBT Components
CBT for Behavioral Medicine typically includes the following parts.
- Self-monitoring
- Activity-rest pacing and behavioral activation
- Cognitive restructuring
- Problem-solving
- Relaxation and mindfulness training
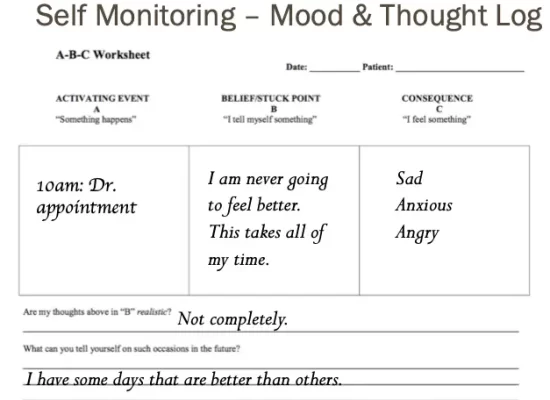
1. Self-Monitoring
CBT generally involves daily “homework assignments” that are completed outside of sessions. During this initial assessment phase, self-monitoring in the form of diary keeping often occurs. Examples of this might be recording mood, problem behaviors, or thoughts associated with moods, as is the case of this example.
In a mood and thought log, we begin to better understand the association between our thoughts and mood. This kind of log can also help us to better understand patterns in thinking and mood.
In a patient with a chronic illness, self-monitoring can also include collecting information to help with medical management, such as keeping a diary of physical symptom severity or pain.
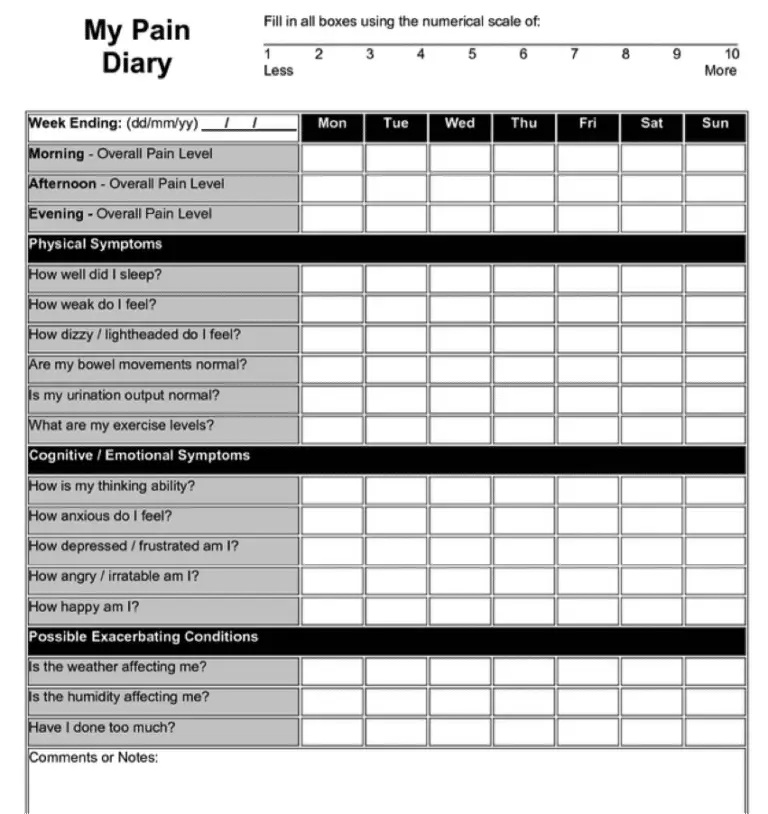
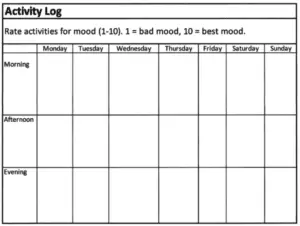
With the type of log below, we are working to understand the relationship between our mood and activities. It can also help us to challenge mood dependent memories. For example, research shows that if we are depressed, we are more likely to remember negative events from our week. With the aid of this type of a log, we can readjust that false belief, allowing ourselves to pay attention to more positive activities. It can also help by assisting one to clearly see the more positive activities that occurred in a week. Finally, this type of log can help us to determine if restarting positive activities are helpful.
2. Activity-Rest Pacing and Behavioral Activation
‘Pacing’ is the practice of balancing activity and rest to manage chronic illness and pain, or “energy management, with the aim of maximizing cognitive and physical activity, while avoiding setbacks/relapses due to overexertion.” With planned periods of rest and activity, one is able to regain control over difficulties resulting from illness or pain, and gradually increase physical and pleasurable activities.
3. Cognitive Restructuring
Automatic thoughts are the thoughts that come to our mind so automatically that we are most often not even aware of them. They are happening all the time, and they are changing all the time.
For example, we all know that feeling of being late for an appointment (or maybe just fearing you will be). In this situation, we say to ourselves a stream of painful thoughts:
- “My co-workers are going to be mad at me.”
- “I shouldn’t have stopped for lunch.”
- “I am going to be fired.”
- “I am a failure at everything.”
What we know is these types of thoughts can be extreme in those with chronic difficulties, and when we learn to adjust these thoughts with more rational, more balanced, and more accurate thoughts, we feel less distressed. Imagine how we would feel if we instead said to ourselves:
- “I have not been late before and they are likely to understand.”
- “This was something I could not have planned for.”
- “I have held this job for 5 years successfully.”
4. Problem-Solving
In this phase we work on problem-solving skills by first learning to recognize when you are having difficulty completing a task, are starting to feel overwhelmed, or avoiding difficulties. Because chronic illness and chronic pain presents many new challenges that need to be problem-solved for, this phase can be extremely helpful.
Once the problems are identified, it is helpful to work to evaluate the pros and cons of a situation, and after weighting these, implement a solution that is broken down into manageable smaller tasks.
In this phase, we pay particular attention to procrastination and avoidance, as these two help to maintain the problem and our anxiety related to the problem.
5. Relaxation and Mindfulness Training
In this phase, we learn relaxation strategies like diaphragmatic breathing and progressive muscle, and mindfulness strategies. Both relaxation and mindfulness have been shown to reduce psychological distress related to chronic illness and pain.
Finding the right therapist
Behavioral medicine is a specialized discipline, and many therapists are not trained to provide psychotherapy within this framework. Dr. Pereira of St. Kitts Counseling Services is trained and experienced in providing behavioral health techniques for chronic illness and pain.
Contact Dr. Pereira
Contact Dr. Pereira at (869) 668-4646 to discuss your difficulties or to schedule an appointment. Call today to get started feeling better.